The Tip Of The Iceberg: Celiac Disease
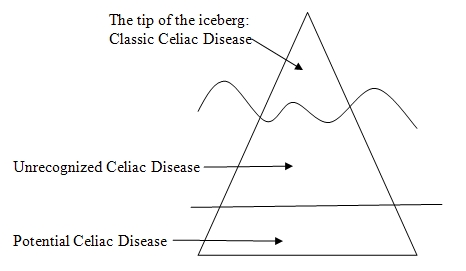
Physicians used to be taught that celiac disease was a rare condition that should only be considered in people with severe diarrhea, abdominal pain and weight loss. It was not diagnosed often. Because of the small number of people with the diagnosis, those with gluten intolerance did not have readily available support groups or places to easily find gluten-free food.
Celiac disease is now being diagnosed much more frequently. It is believed that about 1% of people of European descent have celiac disease. It is not as common in individuals who come from areas where wheat is not a staple of the diet. For example, it is less common in Asians.
There are a number of reasons why celiac disease is being diagnosed more frequently. One is that doctors have learned that it is not as rare as they used to believe. Another is that doctors are screening people who are at risk for having celiac disease but do not have symptoms. Celiac disease is associated with a lot of other so-called “autoimmune” diseases. Doctors will consider looking for celiac disease in patients with insulin-dependent diabetes, for example, or low thyroid, even if they have no intestinal problems. Doctors also screen relatives of patients with celiac disease because they are more likely to have it.
This is made much easier because there are good blood tests that can find a lot of the cases of celiac disease. These are the tests for antibodies to tissue transglutaminase [tTG] or endomysial [EMA], tests which are performed on blood samples. People who have these antibodies still need an intestinal biopsy to confirm celiac disease.
Because doctors are screening people at risk, they are finding individuals with celiac disease who have few or no symptoms. Very young children usually do have diarrhea and what is called “failure to thrive” which means they are not growing. Older children and teenagers may not have these symptoms. People in general who are at high risk and are screened may not have typical symptoms. For example, as many as three quarters of people with diabetes who do turn out to have celiac disease have no gastrointestinal symptoms at all.
Since the tendency toward celiac disease is inherited, there is a large group of people with the potential to have the disease. However, the genetic part is not enough. Something else happens that allows gluten to get into areas in the intestine where it can cause damage. This may be something like a couple of cases of “stomach flu.” Also, to have celiac disease, a person needs to be exposed to enough gluten.
After these events have happened to susceptible individuals, they may have a period of time when some amount of damage is occurring in the small intestine, but they don’t have symptoms. Or if they do have symptoms, they are not serious enough to call attention to the real problem.
There are many unanswered questions. Do all patients with unrecognized celiac disease need to be found? Getting a diagnosis means being told to eat a gluten-free diet forever. This is good because it prevents intestinal damage and other consequences. It’s important to make the diagnosis as early as possible in children.
On the other hand, there have been studies that show that not all of these individuals ever have symptoms, or an increased chance of severe illness or death. This is especially true in older people. They can have celiac antibodies, but never develop obvious celiac disease. People over 50 years of age with the antibodies may not have any serious health problems without treatment except for a tendency toward weak bones (osteoporosis).
Doctors working in this field have questioned whether or not giving older people with “silent” or unrecognized celiac disease the diagnosis would improve or worsen their quality of life.
Research in this area will continue. At this time, doctors have to decide who to screen, because there are no set guidelines or any public health policy dictating who to screen or when to screen. Individuals who believe they or their family members are at risk for celiac disease should certainly discuss this with their doctors and ask for testing.
[hr]
References:
Morbidity and mortality among older individuals with undiagnosed celiac disease. Gastroenterology. 2010 Sep; 139(3):763-9.
Celiac Disease Among Children and Adolescents. Current Problems in Pediatric & Adolescent Health Care. 2007; 37:86-105 (diagram adapted from this article).






